5 Reasons Why BMI is Totally Bonkers
The Body Mass Index (commonly referred to as the BMI) has become the primary way that doctors and other healthcare professionals decide whether or not we are “healthy.” If you’re in the “overweight” or “obese” category, you’re automatically told you need to lose weight. But is this actually correct advice? Read on the learn more about the (many, many) problems with using the BMI as a measure of health.
This post is an edited excerpt from my new book, Unapologetic Eating: Make Peace with Food and Transform Your Life.
If you’d like a copy of this blog as a PDF download, you can download a copy here.
The History of the BMI
BMI is a measure of your weight compared to your height (specifically, it calculates kilograms of body weight per meter squared of height). While the BMI is widely used to categorize health status and disease risk, the original inventor didn’t set out to measure health at all.
In 1832 a Belgian astronomer and statistician named Adolph Quetelet developed something called the Quetelet Index (QI), which was the ratio of a person’s weight in kilograms to their height in square meters. He developed the QI to categorize a population of human beings and to define the characteristics of a “normal man.” Quetelet had no interest in measuring health or “obesity”; he was a statistician looking at population models rather than a medical practitioner studying individual human health conditions.
Most importantly: he developed the QI using data exclusively from a white, European, male population. This means that it didn’t take into account body sizes and diversity in other populations and ethnicities. Nevertheless, the QI eventually became what we know today as the BMI.
Fast forward to the early 1900s in the United States, where diet culture (rooted in racism, classism, and female obedience) had a firm foothold, and people were starting to ask doctors to help them lose weight. At the same time, U.S. life insurance companies observed a higher rate of death for people (again white, wealthy men) who were “overweight” using a ratio of weight and height that they developed into weight tables.
Later research, which included much larger and more diverse samples of the population, showed that there was actually lower mortality in people who were “overweight”. Despite this new data, insurance companies took their early data and, to save their private companies money, promoted weight as a determinant of early death.
At this point, BMI was still not intended to be used to evaluate a person’s health. However, in 1972 researcher Ancel Keys, who disagreed with the insurance weight tables and sought to find a different way to evaluate body mass, proposed that the Quetelet Index now be called the Body Mass Index (BMI) and that it be used to study and link health, disease, and “obesity.” This brings us to the measurement that is still widely known and used today.
The Problem(s) with the BMI
BMI has been widely recognized as a problematic measurement for several reasons:
1. The BMI was developed by a Belgian astronomer and statistician (not a health researcher or medical professional) who was studying groups of white men, not looking at individuals and their health outcomes.
2. It is based on height and weight data taken primarily from white, middle- to upper-class Europeans, which means it’s not a representative sample of the general population and does not account for differences in “average” body sizes in other ethnic groups.
3. BMI does not take into account age, sex, body frame, body composition, fat distribution, or how muscle mass changes with age. For example, people who have a high percentage of muscle mass end up being classified as “overweight” or “obese,” even if they have low amounts of body fat.
4. The differences between BMI classifications—i.e., between “normal” weight and “overweight” or “obese”—are largely arbitrary. They are not based upon any scientific data but defined instead by a handful of people with ideas of what a “normal” weight should be. For example: a few decades ago, the “normal” weight BMI cutoff was lowered in response to a report funded by pharmaceutical companies that make weight loss drugs. Overnight, millions of people went to bed a “normal” weight and woke up “overweight”. (More on this below)
5. BMI assumes we know someone’s behaviors and health status based purely on their body size. However, there is much individual variability based on factors like age, ethnicity, body composition, and social factors (which account for the majority of health outcomes). When we actually look at the data, we can see that BMI is NOT a good indicator of health status:
- People who are classified as “overweight” have a lower risk of death than any other group.1
- People with BMIs of 30-34.9 (in the “obese” range) have the same risk of death as those with “normal” BMIs.1
- The highest death risk is actually among people in the “underweight” BMI category.2
- One third of people classified as “obese” would be classified as “healthy” while nearly one third of people in the “normal” weight BMI category would be classified as “unhealthy.”3
- Those with “obese” BMIs living with type 2 diabetes, high blood pressure, cardiovascular disease, and chronic kidney disease live longer than thinner folks with these conditions.4
Not to mention, labeling people with “overweight” and “obese” BMIs as “unhealthy” leads to discrimination and shame, which do not motivate people to make better lifestyle choices.
The table below is a standard BMI chart with classifications.
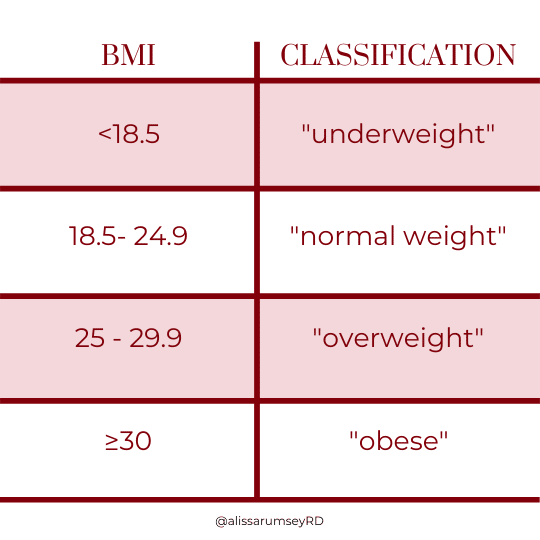
*See the note below for why I put the words above in quotes
How Are The BMI Categories Decided?
So glad you asked. While many health professionals (including myself once upon a time) use BMI to assess for health risk or health status, the cutoff points between BMI categories (i.e. “Normal” vs. “Overweight”) are not based on any scientific data – they were arbitrarily decided.
In 1998, the National Institutes of Health (NIH) decided to lower the “overweight” BMI category threshold to 25 for all genders. Previously, it had been 28 for men and 27 for women. The committee based this decision on a World Health Organization (WHO) report from 1996, which was written by the International Obesity Task Force (IOTF), which recommended the BMI category of “overweight” be lowered.
The primary funders of the IOTF report? Hoffmann-La Roche and Abbott Laboratories, two pharmaceutical companies that make weight-loss drugs. That’s right, the report dictating that certain people who were previously said to be “normal weight” be now considered “overweight,” was funded by companies that were selling weight-loss drugs. Talk about a conflict of interest!
Not to mention that various weight-loss drug companies were paying many of the researchers and scientists who were on the WHO and NIH committees. These companies had an active interest in having more Americans classified as “overweight” so that they would have a much larger market for their weight-loss drugs.
The “Obesity Paradox”
Aside from BMI misrepresenting the health of many people, the assumptions made about those in different categories are actually scientifically inaccurate. This is a phenomenon known as the “obesity paradox.”
Note: It’s only considered a “paradox” because researchers, with their weight bias, expected the opposite to be true.
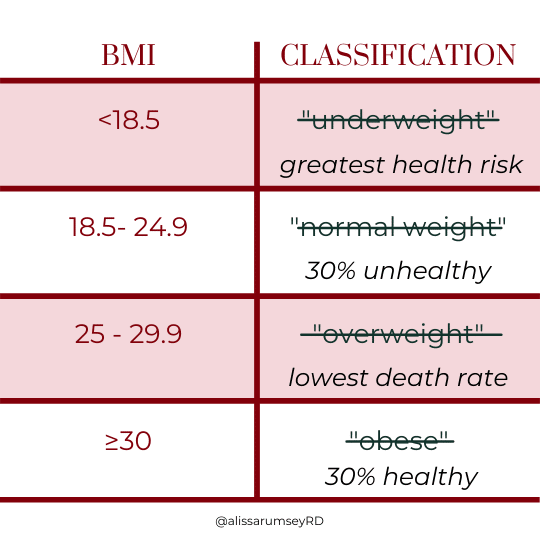
A large-scale study (40,000 people) done less than five years ago found that nearly half of people classified as “overweight” and one-third of people classified as “obese” are actually metabolically healthy (meaning they have normal labs such as blood pressure, cholesterol, and blood sugar, indicating good overall health).3
In addition, nearly one-third of people in the “normal” weight BMI category were found to be metabolically unhealthy.5, 6 (Warning: stigmatizing language in these studies) There is not one disease that only affects people at higher weights. People of all shapes and sizes are affected by the health conditions – it’s only people at higher weights who have these diseases blamed on their body size (see how hypocritical this is?).
In terms of groups of people, we see the highest death risk among people who are in the “underweight” BMI category, and the lowest risk of death is people in the “overweight” BMI category.2 That’s right: people who are “overweight” have a lower risk of death than people who have a “normal” BMI. How’s that for a paradox?
In addition, people with BMIs of 30-34.9 (in the “obese” range) have the same risk of death as those with “normal” BMIs.1
Furthermore, those with “obese” BMIs living with type 2 diabetes, high blood pressure, cardiovascular disease, and chronic kidney disease live longer than thinner folks with these same conditions.7, 8 Weight also seems to have some protective effect as we age, with research finding that in people older than age 55, those with a BMI in the “overweight” and “obese” categories had decreased risk of death compared to people with “normal” and “underweight” BMIs.
A great overview of the current weight science is this paper by Jeffrey Hunger, Joslyn Smith, and Janet Tomiyama.
The re-imagined BMI chart below, a new BMI chart if you will, might help shift people’s assumptions:
A Note About The Terms “Obese” and “Overweight”
You’ll notice that I put the words obese and overweight in quotes. While these words are commonly used to describe larger bodies, they are words that have been developed and co-opted by the medical community to medicalize and pathologize a person’s body (which means “to represent something as a disease” or treat someone as if they are abnormal).
“Overweight” is a word that assumes that there is a “correct” weight that a body should be and that if you are “over” that weight, then you are abnormal or different. The word overweight is rooted in the BMI charts (which, as you just learned, is flawed and deeply problematic).
The word “obese” comes from the Latin word obesus, meaning “having eaten until fat.” The term assigns illness based on size, not on any other parameter, and places blame on the individual, which is not only incorrect but is stigmatizing and can cause stress, anxiety, and shame.
When we label people as “overweight” or “obese,” we are labeling them as abnormal or unnatural and pathologizing their body as “a problem”. In doing so, we are marginalizing them. These are words that can cause stress, anxiety, and deep shame – none of which motivates positive behavior change.
The Harm of Categorizing People Using BMI
Let’s take a moment to think about how pathologizing people’s bodies (aka labeling them as abnormal) has contributed to harm. Once someone’s body size is labeled as problematic, the assumption is that the person is making poor lifestyle choices and that showing them they have a “problem” will motivate them to change. Aside from this not being an effective motivator, it actually perpetuates mistreatment of people in larger bodies.
Below are some examples of weight-based discrimination and bias:
- People who have an “obese” BMI make less money than thin people and are less likely to get promoted.
- The average American woman is a size 14—and 67 percent of American women wear a size 14 or larger—but most retail clothing stores don’t carry anything larger than a size 12.
- Fat jokes are considered socially acceptable.
- People in larger bodies pay more for many goods and services, like airline tickets, insurance, and clothing.
- Kids are routinely shamed and bullied by other children as well as by teachers and family members.
- People assume that someone who is “obese” doesn’t eat healthy or exercise.
- It’s considered a “kindness” to compliment someone on their weight loss and tell them how great they look “now.”
Ultimately, rather than wondering: what is the problem with my body? can we shift the question to:
- What is the problem with how my body is seen and treated?
- What is the problem with using the BMI to categorize human’s health status?
Bottom Line:
It’s time to stop making assumptions about people (and on ourselves) based on body size. We need to collectively move away from using BMI whenever possible. We can encourage people to decline being weighed at doctor’s appointments (YES this is something that is well within your right to do – Regan Chastain has a series of helpful posts on her blog here and here).
If you are looking to improve your health (or you are a health professional helping others improve their health) – try to move away from using weight or BMI to dictate “how you are doing”. Instead, look at your health behaviors from a curious, non-judgmental, self-compassionate place. For example, you may look at how aware you are of your hunger and fullness cues, your energy level, sleep habits, stress coping mechanisms, binging frequency, food cravings, and/or improvements in flexibility, strength, or endurance.
A dietitian well-versed in the weight-inclusive approach can help you prioritize your health behaviors and help you define for yourself what “health” looks like for you. Ultimately, it is up to you if you want to pursue health and – either way – no one should be treated differently because of how much they weigh.
This blog contains edited excerpts of my new book, Unapologetic Eating: Make Peace with Food and Transform Your Life.
Looking for more support?
Check out my Unapologetic Eating 101 Course, an online, self-paced program to liberate yourself from dieting and make peace with food and your body.
My team and I also offer virtual one-on-one nutrition coaching support to help people liberate themselves from dieting and make peace with food and their bodies.
Author Bio
This post was compiled and written by Autumn Rauchwerk, a dietetic intern and Registered Yoga Teacher living in Brooklyn, New York. Follow her on Instagram (@autumnrosewellness) or on her website to learn more and join her for free and donation-based virtual yoga classes.
The post was reviewed by Alissa Rumsey, MS, RD, CSCS, a registered dietitian and Certified Intuitive Eating Counselor. She specializes in weight-inclusive care, intuitive eating, body image healing, mindfulness, self-compassion, and healing from chronic dieting, disordered eating, and eating disorders. Alissa holds a Bachelor’s Degree in Nutrition and Exercise Science, and a Master’s Degree in Health Communications, and is also an NSCA Certified Strength and Conditioning Specialist.
6 Comments
Leave a Comment
share the love

about
Alissa Rumsey, RD.
Alissa Rumsey, MS, RD, CDN, CSCS (pronouns she/her/hers) is a registered
dietitian, nutrition therapist, certified intuitive eating counselor, and the author of
Unapologetic Eating: Make Peace With Food and Transform Your Life. Alissa is
passionate about helping people reclaim the space to eat and live,
unapologetically.
A twice-a-month round-up of inspirational stories, lessons, practical tips and encouragement for living your most authentic, unapologetic life.
The Unapologetic Life
RECENT POSTS
The Unapologetic Life
A twice-a-month round-up of inspirational stories, lessons, practical tips and encouragement for living your most authentic, unapologetic life.








Alissa, thank you for this post! Illuminating to say the least.
My pleasure Traci, thanks so much for sharing this 🙂
Alissa, I just happened to stumble across your column and I was glad I did. What you are saying is what I have been saying for years that the BMI has been adjusted as a one-size-fits-all and is not realistic. Thanks for confirming what I thought all along. My doctor looks at my chart and he’s one of them that thinks the BMI is the Bible., he shakes his head, and he goes you’re healthy. I reply yes, I know. so thanks for kind of confirming what I knew all along that it was BS or at least that you cannot use it as a one size fits all
Thanks so much for sharing your story Mike! I’m glad the post was validating to your experience.
20 years ago, as a teenager, a stupid chart told me I was “overweight”, making me feel ugly, unworthy and powerless. Now you are telling me that I am actually part of the population with the lowest mortality risk!
It makes me so angry to realize how much and for how long diet culture lied to me, to all of us. It took away years of my life. Thank you so much for everything you are doing to educate and awaken people to the truth.
Thanks for sharing, Luna – I’m so sorry this happened to you, your anger is completely understandable. I’m glad you found this helpful!