Is Weight Really the Problem?
If you care about your health and the health of those around you, it might be a good time to ask yourself: Is weight really the problem? Read on to better understand where our focus on weight comes from (and no, it’s not for the health, wellbeing, or self-confidence reasons that you may think) plus learn about the negative consequences that can come when you put the focus on weight. You’ll begin to better understand the myriad of other factors that play into health and how you may benefit from approaching things differently.
This post is an edited excerpt from my new book, Unapologetic Eating: Make Peace with Food and Transform Your Life.
If you’d like a copy of this blog as a PDF download, you can download a copy here.
The Biased Roots of the Cultural Desire to Lose Weight
Nowadays, it’s easy to assume that the link between health and weight has always existed. Certainly that’s what most health professionals teach and what’s disseminated through the media. But interestingly enough, the roots of people’s desire to lose weight predate any scientific “evidence” connecting weight and health.
When the medical community started advising weight loss for their patients in the early 1900’s, there was no scientific evidence linking weight to health (and, as you’ll see shortly, there’s still very little to go on). The societal desire for thinness, and bias against fatness – or fatphobia – came first. When the medical community started to advise weight loss it wasn’t because there was any scientific evidence linking weight to health, but because our culture had already created a desire for thinness and a bias against fatness.
Our culture equates thinness to health, happiness, attractiveness, and worthiness, a system of beliefs that is often referred to as diet culture. To be thin is to be deemed morally superior, whereas to be fat is to be seen as unhealthy, lazy, and a failure. In this way, our culture promotes dieting and weight loss as a way to achieve a higher status and worthiness. We’re told that we have to eat a certain way and be a certain size to be “healthy.” Therefore, certain foods and certain body types are inherently elevated, while others are vilified.
These cultural beliefs about body size and morality, worthiness, and even health didn’t come from nowhere. They were specifically created to establish social hierarchies and control people.
Colonialist, Racist & Sexist Origins
Western culture was built upon the control of Black, Indigenous and People of Color, which allowed white people to rise to the top and hold the power. To establish social hierarchies where white people (especially white men) could remain at the top, white Europeans and Americans linked being Black and/or being fat to negative traits like greediness and laziness. White men effectively created a societal “other,” marginalizing Black people and, in their efforts to do so, relegated fatness as something to fear and avoid. This fatphobia, rather than any concern for health or well-being, is what began our culture’s fixation on weight.
In addition to colonialism and racism, diet culture also has its roots in sexism and the desire for female obedience. We live in a patriarchal society, a social system in which men hold the majority of the power and have historically dominated leadership roles at every level of society. So, who benefits from women being preoccupied with dieting and conforming to body ideals? Men (white men in particular).
By creating a set of body ideals, these groups of people – notably women, people of color, and fat folks – internalized the message that they couldn’t trust themselves. Obsessing about weight, size, and appearance was an effective way to hold women back in society and keep their attention on meeting these aesthetic “ideals” rather than focusing on their political, social, or economic ambition.
As Naomi Wolf describes in her book The Beauty Myth, “A cultural fixation on female thinness is not an obsession about female beauty but an obsession about female obedience … Dieting is the most potent political sedative in women’s history; a quietly mad population is a tractable one.” Once again, society’s emphasis on thinness is not about health or well-being but about the submission and control of groups of people.
Weight Is Not a Good Indicator For Health
Despite what you may have been taught or told, weight is not a good indicator of health. There is zero research that proves that higher amounts of weight or body fat cause diseases like heart disease, cancer, or diabetes. While some of these health conditions are more common in people at higher weights, and there may be a correlation between weight and health, this is not the same thing as causation.
So what about all this research that links weight and health? Well, when researchers and health professionals started studying health and weight, they already had a bias for thinness and against fatness which is evident when you look at the studies (more on this type of weight stigma below). For example, consider the Body Mass Index or BMI. In 1998, the National Institute of Health decided to lower the “overweight” BMI category from 27 for women and 28 for men to 25 for both genders. Overnight, millions of people became “overweight”.
Why did they do that you ask? The decision was based on a report funded by pharmaceutical companies that make weight loss drugs. See the conflict of interest there? If more people – and more doctors – thought they were “overweight”, and need to lose weight “for health”, then they could sell more drugs. This occurred again in 2013 when the American Medical Association decided to classify “obesity” as a disease. This time they went against their own committee’s recommendation, who found that there was no scientific evidence to show that higher body weight caused health issues.
Weight isn’t the underlying cause for poor health; it may simply be an effect of other variables that are the actual causes of disease, such as genetics, social and environmental factors, weight stigma, and behaviors like diet and exercise. Yet in our weight-centric society, “weight loss” is often prescribed as the way to achieve health and well-being.
Want to better understand the BMI and all its problems? Check out my post 5 Reasons Why BMI is Totally Bonkers.
Weight Stigma Matters MORE Than Weight
Weight stigma is discrimination or stereotyping based on someone’s weight, encompassing negative attitudes and beliefs about people in larger bodies and assumptions made about them based on the size of their bodies. These include beliefs such as fat people are lazy, sloppy, uneducated, and/or unattractive – that they have somehow “earned” their fatness or the discrimination enacted upon them. Weight stigma is found in the workplace, in schools and universities, in health care facilities, with members of the community, at restaurants, in stores, and in interactions with friends and family. The media perpetuates weight stigma and fatphobia to the point where it’s been so normalized that most people don’t even recognize it as a problem.
Other examples of weight stigma include:
- “Fat jokes” are considered socially acceptable
- Having to pay more for many goods and services, like airline tickets, insurance, and clothing.
- A doctor telling someone who comes in for a sore throat that they need to lose weight
- People in larger bodies making less money than people in thinner bodies
- Someone being told by friends and family that they would be healthier and happier if they lost some weight
- Despite the fact that 67% of women wear a size 14 or above, most retail clothing stores doing carry anything above a size 12
While there is no evidence that weight causes adverse health consequences, there is evidence tos how that weight stigma causes a wide variety of health problems. When someone is teased, excluded, demeaned, or blamed for their weight, regardless of how much they actually weigh, they experience an increase in stress. The chronic stress weight stigma causes is extremely problematic for people’s bodies and health. Experiencing weight stigma contributes to increased blood pressure, chronic inflammation, diabetes, cardiovascular disease, anxiety, depression, low self-esteem, and disordered eating behaviors.
The more someone experiences weight stigma, the more likely they may be to internalize these messages and have bias and stigma towards themselves. This internalized stigma then causes further mental and physical health repercussions.
Another way weight stigma contributes to health consequences is that many people at higher weights avoid going to the doctor because of a fear of experiencing stigma. They then end up missing out on proper medical care when needed. Studies have shown high levels of weight bias among medical professionals (including dietitians) which leads to worse care for fat people and poorer health outcomes. For patients with higher BMI’s, doctor’s spend less time with the person, have less patience with them, take them less seriously, provide less health education, and are less likely to perform certain interventions and screenings including pelvic exams, mammograms, and cancer screens (compared with thinner patients)1, 2.
Healthcare providers think they are doing patients a favor by giving weight-related feedback, that they are helping their patients. However, what research has actually found is that when people receive weight-related feedback they are less likely to make long-term health behavior changes. When they experience weight stigma, their eating and exercise behaviors get worse.
When thinking about health, it is easy to focus solely on physical health, while mental and emotional health are often overlooked. Dieting and weight-centric approaches to health (in which weight is seen as a primary indicator of health) can adversely affect mental health, and we see increased anxiety and depression and lowered self-esteem and self-confidence.
This might be a good time to re-examine the question: is weight really a problem? Or is our laser focus on weight the bigger issue?
A Different Framework for Health
When we think of modifiable health risk factors (i.e those that we have control over), our behaviors – not our weight – has the biggest impact on health. It is important to remember that weight is not a behavior; it is not something that we have that much control over all things considered. Eating nutritious foods and moving more positively impact markers like blood sugar, heart rate, and blood pressure even without any weight loss (there is lots of research to support this).
The challenge is that, because of the widespread emphasis on weight and weight loss for health above all else, when people make beneficial behavior changes and don’t see weight loss, they think that what they are doing isn’t working and then they stop practicing these beneficial behaviors.
Instead of using weight, physical health can be measured using cholesterol levels, blood pressure, blood glucose, and insulin levels.
In addition to some of these markers, you can often get a better understanding of “how you’re doing” based upon how you feel physically, mentally, and emotionally. For example, some of the ways in which my clients and I measure their health progress include:
- Being more attuned to their body’s hunger and fullness cues.
- Not stressing about food as much and constantly thinking about what to eat (or not eat).
- Having more energy.
- Improved sleep quality and quantity.
- Finding more ways to cope with stress and other emotions.
- Less frequent binging behaviors.
- A decrease in food cravings.
- More body trust and less second-guessing food choices.
- Improved flexibility, strength and/or endurance.
Health at Every Size® (HAES®)
One approach that can be useful in this scenario is the Health at Every Size® framework (also known as HAES® which is a registered trademark of the Association for Size Diversity and Health). HAES® is a weight inclusive, anti-diet approach that offers an alternative to the weight-centric model of care.
It rejects using weight or BMI as a proxy for health and supports people of all sizes finding compassionate ways to take care of themselves no matter what their size. The focus remains on health, rather than weight, and promotes positive physical and mental health behaviors through the five principles:
- Weight inclusivity
- Health enhancement
- Respectful care
- Eating for well-being
- Life-enhancing movement
HAES® emphasizes acceptance and respect of inherent body size diversity, promotes health policies giving better access to care, works to end weight stigma, promotes intuitive eating that is flexible and based on internal signals, and encourages people to find enjoyable movement practices. This approach has been extensively researched is associated with a multitude of health benefits, including improved cholesterol levels, lower blood pressure, no weight cycling, better body image, and increased physical activity (all independent of weight changes).
Social Determinants of Health
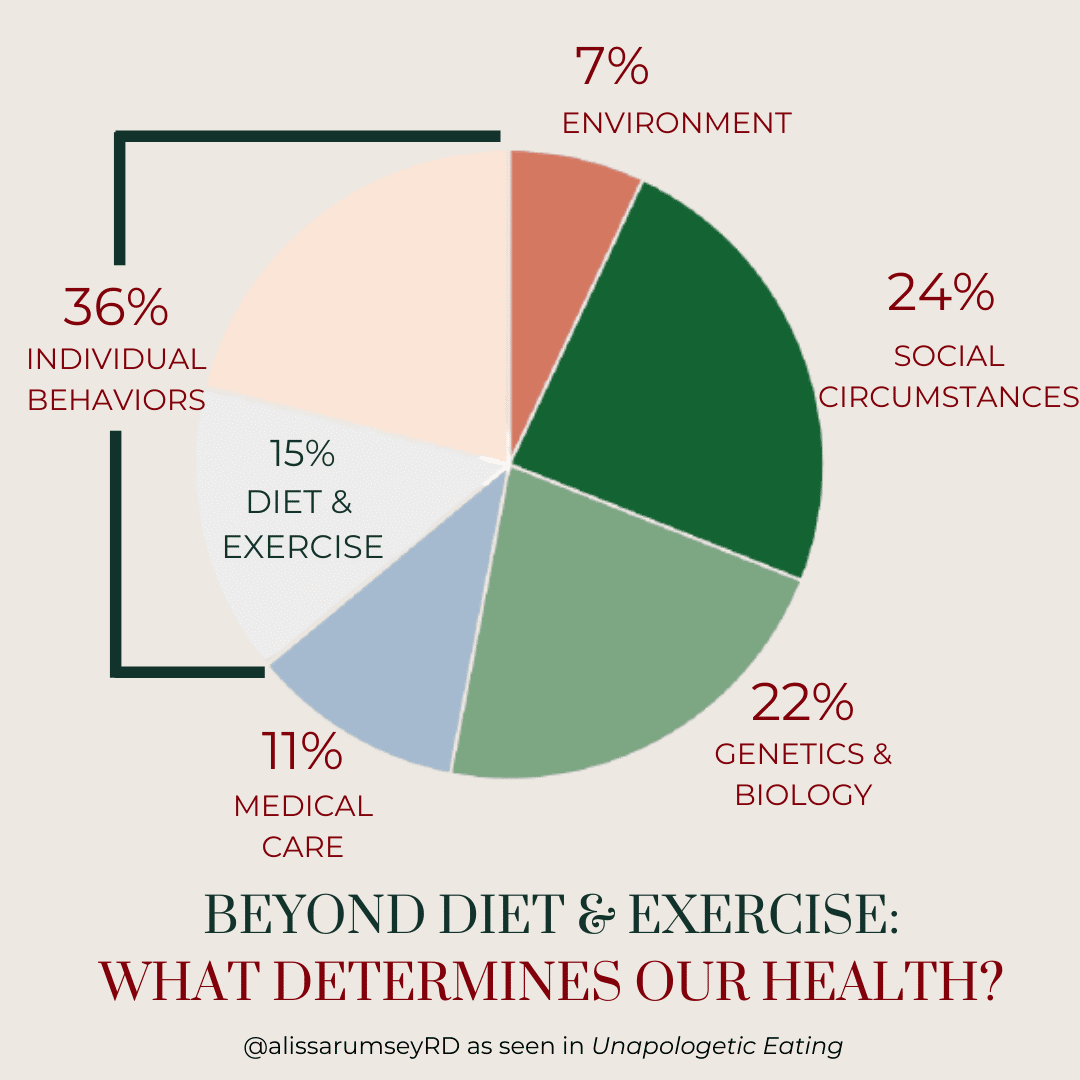
For the most comprehensive view of health as a whole, we must talk about the social determinants of health, which determine about 89% of health outcomes. According to the World Health Organization, the social determinants of health are “the conditions under which people are born, grow, live, work and age.” The other 11% of health is determined medical care – access, quality, patient engagement, and health literacy. In thinking about health this way, it becomes obvious that so much of health is outside of our control. Think about the below factors that determine health and how little personal control many of us have over them:
- Genetics
- Pollution exposure
- Adequate food and clean water access
- Access to safe and reliable housing and transportation
- Type of job and working conditions
- Education level
- Income level
- Access to medical care
- Stress levels
- Gender identity & sexual orientation
- Facing discrimination (like weight stigma and racism)
- Social support and coping skills
- Language and literacy
Individual health or lifestyle behaviors – of which diet and exercise are a part – make up only about 36% of the differences in health that we see between groups of people. These behaviors include diet and exercise, yes, but also things like cigarette use, alcohol use, drug use, and safety behaviors like wearing a seatbelt. This means that diet and exercise make up only about 15% of our health outcomes.
The chart* below depicts the factors that influence health, many of which are themselves influenced by social circumstances rather than individual choice. *Inspired by this chart by GoInvo
Health improves in line with a person’s socioeconomic status, meaning the more money, power, and resources a person has, the better their health. If you make enough money to support your basic needs, have access to safe housing, education, and good healthcare, and you don’t experience oppression or discrimination on a regular basis, then you are much more likely to have better health outcomes.
On the other hand, if you make less income, live in an unsafe neighborhood, and/or face regular discrimination, this will increase your stress levels. When an acute stress response is turned on briefly, it can save your life (think running from a tiger or dodging a bullet). But when that stress response becomes chronic, and is activated day over day for years on end, it increases a person’s risk for a whole host of diseases.
For example, Black Americans have higher rates of high blood pressure that are not explained by genetics or lifestyle alone, but by their experiences of racism (the American Medical Associate just recently recognized racism as a public health threat). Similarly, people who experience poverty also have increased rates of high blood pressure, much of it related to the impact of stress.
If Not Weight, Then What?
At this point, you may be thinking, “Ok, so weight isn’t necessarily the problem. So what can I do?”
First of all, if you are still struggling with this and still thinking “but I want to/need to lose weight”, that is ok. It makes so much sense why people would want to lose weight. In doing so, we are promised acceptance, belonging, health, and happiness. For the clients I work with, the idea of giving up the idea of losing weight can bring about the (legitimate) fear of being judged, disrespected, cast aside, or worse.
This is why my anti-diet colleagues and I do not shame anyone who attempts to lose weight and conform to our society’s body ideals. Very real oppression exists for people who hold marginalized identities, including women, people of color, and fat folks, so it’s understandable that someone would want to protect themselves from this injustice by losing weight.
As you grapple with this, here are two other ways to consider moving forward:
1. We can work – individually and collectively – to reverse discrimination. We can stop talking about the size of people’s bodies. We can work to educate ourselves on the intersection of discrimination based on race, gender, and sexual orientation, with weight-based discrimination. We can question our assumptions and inherent biases. We can pause before trusting our assumptions and work to unravel where they are coming from.
A great place to start is reading the book Fearing the Black Body by Sabrina Strings. Here are some more resources to help you get started.
2. We can measure health progress differently. Instead of basing “health” or “progress” on weight, BMI, or body size, we can measure our health and wellbeing progress on other factors (more specifics on this in the ‘A Different Framework for Health’ section above). We can look at attunement with hunger and fullness cues, energy levels, sleep habits, emotional coping mechanisms, binging frequency, food cravings, and improvements in flexibility, strength, and/or endurance.
For more ideas, check out this post: 23 Ways to Measure Progress Without Stepping on a Scale.
This blog contains edited excerpts of my new book, Unapologetic Eating: Make Peace with Food and Transform Your Life.
Looking for more support?
Check out my Unapologetic Eating 101 Course, an online, self-paced program to liberate yourself from dieting and make peace with food and your body.
My team and I also offer virtual one-on-one support – you can check out our virtual intuitive eating nutrition coaching packages.
My book, Unapologetic Eating: Make Peace with Food and Transform Your Life, is also a great resource that includes information, research, and reflection prompts to help you move away from dieting and come back home to your body, so you can live your most unapologetic, liberated life.
Author Bio
This post was compiled and written by Autumn Rauchwerk, a dietetic intern and Registered Yoga Teacher living in Brooklyn, New York. Follow her on Instagram (@autumnrosewellness) or on her website to learn more and join her for free and donation-based virtual yoga classes.
The post was reviewed by Alissa Rumsey, MS, RD, CSCS, a registered dietitian and Certified Intuitive Eating Counselor. She specializes in weight-inclusive care, intuitive eating, body image healing, mindfulness, self-compassion, and healing from chronic dieting, disordered eating, and eating disorders. Alissa holds a Bachelor’s Degree in Nutrition and Exercise Science, and a Master’s Degree in Health Communications, and is also an NSCA Certified Strength and Conditioning Specialist.
5 Comments
Leave a Comment
share the love

about
Alissa Rumsey, RD.
Alissa Rumsey, MS, RD, CDN, CSCS (pronouns she/her/hers) is a registered
dietitian, nutrition therapist, certified intuitive eating counselor, and the author of
Unapologetic Eating: Make Peace With Food and Transform Your Life. Alissa is
passionate about helping people reclaim the space to eat and live,
unapologetically.
A twice-a-month round-up of inspirational stories, lessons, practical tips and encouragement for living your most authentic, unapologetic life.
The Unapologetic Life
RECENT POSTS
The Unapologetic Life
A twice-a-month round-up of inspirational stories, lessons, practical tips and encouragement for living your most authentic, unapologetic life.








Excellent article, as usual, with some well presented points that I have never considered.
I am an RD and have taken the Height/Weight question off of my intake forms. Keep us the good work.
Thanks so much Barbara! I appreciate you sharing your feedback 🙂
I absolutely loved Fearing the Black Body, and will definitely check out The Beauty Myth that you mentioned in this post. It’s wonderful to see other RDs also not focusing on weight.
This page is everything and more. I’m currently forming my position statement for my capstone project and was leaning towards something regarding the BMI being outdated or weight not being a good determinate of health.
I look forward to reading more of your material!! Thanks for being an inspiration!
Thank you, Alaina! Good luck with your capstone!